Microdiscectomy

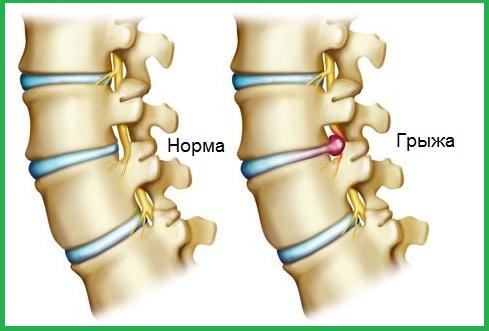

Operation of a discectomy - removal of the intervertebral disc together with a hernia, which causes compression of the nerve, is by far the main surgical method of treating the intervertebral hernia. The very operation of a discectomy is to remove part of the intervertebral disc, which is destroyed by the hernia and protrudes into the lumen of the spinal canal. In addition, during the operation the doctor examines the space between the vertebrae and removes free fragments of the disk from there.
Before performing a discectomy, the doctor can remove a small piece of the affected vertebra - the so-called laminectomy. This operation allows the surgeon to get more access to the vertebra disk.
Currently, surgeons are increasingly resorting to microdiscectomy. This operation is carried out using special operating microscopes. This technique of operation allows you to remove the intervertebral disc through a small incision, thereby not causing injury to surrounding tissues. Usually the operation of a discectomy (or microdiskectomy) is performed under general anesthesia. Operation microdiscectomy is considered more effective in the treatment of pain from the lower extremity (the so-called radiculopathy) than back pain.
Preparation for operation of a discectomy (microdiscectomy)
As with any other operation, discectomy requires preparation. It consists in conducting blood and urine tests, spine examination - MRI or CT. Before the operation, the patient should not eat for 8 hours. In addition, the patient is examined by an anesthesiologist. He chooses the most optimal method of anesthesia, clarifies the patient's presence of chronic heart and lung diseases, as well as allergic reactions to drugs in the past.
Method of microdiscectomy
The microdiscectomy is performed through a 2.5-4 cm incision in the middle in the lumbar region of the spinal column.
Initially, the surgeon lifts the special muscles of the muscles, straightening the back. This muscle does not have to be crossed with a scalpel, as it easily shifts.
After this, the surgeon can already access the spine, removing the membrane over the nerve roots (the so-called yellow ligament). In order to see the nerve roots, an operating microscope is used.
Often, a small part of the inner surface of the facet joint is removed to facilitate access to the nerve root and eliminate pressure on the nerve.
Next, the nerve root gently moves aside and the tissue of the intervertebral disc is removed from under the nerve root.
It is important to note the fact that since most joints, ligaments and muscles remain unaffected, the operation of microdiscectomy does not disrupt the mechanical structure of the patient's spine.
Indications for microdiscectomy
Usually, if the pain in the leg of a patient after conservative treatment begins to gradually subside, then it can completely go through 6 to 12 weeks. And if the patient can endure this pain, then it is recommended to postpone surgery for a short period of time to see if the situation will be resolved without surgery.
If conservative therapy does not give any relief, then one must resort to surgery, in order to release the nerve root, squeezed herniated disc. Urgent conduction of discectomy is required only in those cases when the disc herniation is accompanied by a violation of the function of the bladder and intestine (incontinence of urine and feces).
Microdiscectomy is indicated in cases where conservative treatment is ineffective for at least 6 weeks. However, in this case, you should not postpone the operation for a long time (more than 3 - 6 months).
Postoperative period of microdiscectomy
Usually, microdiscectomy can be performed on an outpatient basis, and the patient does not need to stay in the hospital. Some neurosurgeons recommend a restriction in terms of lifting weights, bending the spine for the first 6 weeks after the operation. However, in view of the fact that the mechanics of the spine in the patient after the microdiscectomy remains the same, the patient can calmly return to the previous physical activity right after the operation. In the literature there is evidence that the resolution of the load immediately after surgery does not lead to an increase in the recurrence of disc herniation or complications.
The efficiency of the microdiscectomy operation reaches 90-95%, which means that in 5-10% of patients in the future there may still be recurrence of a herniated disc.
Recurrent herniation of the intervertebral disc may occur immediately after the operation, and several years after it. However, in most cases of recurrence of a hernia, it occurs in the first three months after surgery. In the case of a recurrence of a herniated disc, the revision microdiscectomy is usually as effective as the first operation. However, after a second operation, the risk of recurrence is higher (15-20%).
In patients with multiple recurrences of herniated discs in order to prevent further relapses, surgical intervention such as spinal fusion can be effective. Spondylodesis is the removal of the intervertebral disc and the "fusion" of two adjacent vertebrae, which guarantees in the future the absence of any recurrence of herniated disc. In case the posterior facet joint is not affected and all other criteria are suitable, it is possible to replace the destroyed intervertebral disc with an artificial one. It is believed that the occurrence of recurrence of the herniated disc is not directly related to the level of activity of the patient. Basically it is due to the fact that inside the disk there are spaces in which the fragments of the disk are contained, and they, in turn, can go out.
Unfortunately, with posterior microdiscectomy, only 5% -7% of the intervertebral disc can be removed and most of the disc can not be seen. In addition, the hole that is held in the thickness of the disk (annulotomy), never overgrows on its own, as the fibrous disc has no blood supply. In addition, there are no surgical methods to restore the outer (annular) part of the intervertebral disc.
Complications of discectomy
As with any other surgical intervention, after discectomy and microdiscectomy complications are possible.
Rupture of the spinal cord. This complication can occur in 1-2% of cases and does not affect the results of the operation, however, within a few days the patient is recommended to have a bed rest, so that the shell is overgrown and there is no leakage of the cerebrospinal fluid.
· Damage to the nerve root.
· Violation of the function of the bladder and intestines.
· Bleeding.
· Infectious complications.



