Gonarthrosis


Deforming arthrosis of the knee joint (gonarthrosis, osteoarthrosis of the knee joint) is a degenerative-dystrophic disease of the knee joint. The development of the disease contributes to a constant load on the knee joint. Women are sick about twice as often as men.
It should be noted that arthrosis of the knee joint is a slowly progressing disease. The most common symptoms of osteoarthritis of the knee joint are severe pain. At first, the pains appear after a long walk, when descending the stairs, lifting and carrying weights. Characteristic increase in pain in cold and wet weather. With the passage of time, the pains become stronger, acquire a permanent character.
Develops a reactive, non-microbial inflammatory process of the inner shell of the joint (synovitis). In this case, a sharp exacerbation of pain may occur. The knee joint increases in size, swells. Then the process subsides and resumes again under adverse conditions.
Patients complain of a crunch, a creak in the knee joint. When palpating, the knee joint is painful, the pain increases with an attempt to move the patella.
Gradually, the walking function is limited. The distance that a patient can pass is reduced. The patient is forced to rely on the cane. In the late stage of the disease, as a result of contraction and contraction of the muscles, contractures are formed in which the tibia is bent at the knee joint, depending on the greater or lesser damage to the inner or outer part of the joint, the shin may be tucked inside or out, and the patient can. Ultimately, movements in the knee joint are sharply limited or completely lost.
The diagnosis of gonarthrosis is clarified with the help of X-ray images, ultrasound investigation, if necessary - computer or magnetic resonance imaging.

The diagnosis of gonarthrosis is clarified with the help of X-ray images, ultrasound investigation, if necessary - computer or magnetic resonance imaging.
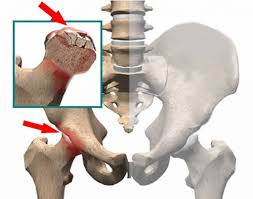
Detect the narrowing of the joint gap. In the initial stages of the disease, the internal or external parts of the joint are usually affected, and the narrowing of the joint gap is observed only on one side. Over time, the process extends to the entire joint. Cartilage bone plate hardens. Bony growths - osteophytes are found at the edges of the articular surface. Ultrasound reveals thinning of hyaline cartilage, chondromalacia, degenerative-dystrophic changes in meniscus and ligamentous apparatus, with synovitis - fluid in the curvatures of the synovial membrane. In arthroscopy, zones of erosion on the articular surfaces of the femur, erect meniscus, hypertrophy of the synovial villus are determined.
Treatment of gonarthrosis (arthrosis of the knee joint) does not differ from the treatment of osteoarthritis of another location. It is recommended to limit the physical load on the joint, but at the same time it is obligatory to practice physical therapy, since the movements performed in the joint allow preserving its mobility and improving the nutrition of the joint elements. Exercises should be chosen with the help of a physiotherapist or physician. Exercise daily. A necessary condition for classes, unloading the knee joint. Those. Exercises are conducted in the position of the patient lying down and sitting. Swimming and swimming are very useful.
If one knee joint is affected, exercise therapy is still prescribed for both joints. Patients are recommended self-massage of the knee joint area, hip and thigh muscles. This also allows improving the blood supply of the joint, maintaining the leg muscles in good condition. To remove the pain syndrome non-steroidal anti-inflammatory drugs, analgesics are prescribed. Various irritating and analgesic ointments are used. Improve blood supply to help vasos-regulating drugs, venotonics. For a long time, drugs are prescribed that improve the condition of articular cartilage – chondroprotective agents. With ineffectiveness of conservative methods of therapy resort to surgical treatment. With relatively preserved function of the joint and the absence of contractures, a small surgical intervention is possible: arthroscopy, using endoscopic technique. The joint is washed, the destroyed fragments of cartilage, menisci are removed, osteophytes are removed. This operation is palliative, but it can improve the function of the joint for 2-3 years if the trauma is low. If there is a predominant lesion of the inner or outer part of the joint, with a slight curvature of the tibia, it is possible to perform an operation called corrective valgus subalgeal osteotomy of the tibia when the internal part of the knee is damaged.
When the external part of the joint is damaged, variciliary supracondylar osteotomy of the femur is performed. Performing this surgical intervention allows you to achieve uniformity of the load on the joint surfaces. With a successful operation, good results are achieved in 85% of patients and the function of the knee joint persists to 10 years. But the main method of treatment is far-gone gonarthrosis, which allows to restore motion in the joint, to return the patient the ability to move and work is the endoprostheses of the knee joint.
Knee replacement involves removing the worn out parts of the bone in your knee joint, and replacing them with metal and plastic parts.
Most often, indications for knee arthroplasty are arthritis or arthrosis of knee joints. Replacement of the knee joint is also reliable and effective, as well as endoprostheses of the hip joint. In most cases, total (full) arthroplasty of the knee joint is made. A partial replacement of the knee joint is less common.
The knee is like a hinge between two bones - the femur of the upper leg (thigh), and the tibia in the lower leg (shin). Usually the heads of these two bones gently slide over each other inside the knee joint. This is possible because they are covered with articular cartilage, a smooth and elastic tissue that covers and protects the heads of bones, allowing them to move one over another easily and painlessly.
All the remaining surfaces inside the knee joint are covered with a thin, smooth tissue called the synovial membrane. The shell produces a special fluid - a synovial fluid that lubricates the joint.
If a disease or injury disrupts the normal operation of the knee, it can cause pain when walking, upright, and also difficulty moving in the knee joint. Most often, the articular cartilage wears or collapses, the hip and tibia begin to rub against each other, which causes pain and mobility disorders.
Indication for endoprostheses of the knee joint is osteoarthritis. As a result of this disease, the knee cartilage becomes thinner, coarser, and in some places completely worn out. Bony growths can also form on the surface of the joint, as a result of which the bones "rub" against each other, which causes pain, swelling and restriction of mobility in the affected knee.
Also indications for prosthetic knee joint are:
· rheumatoid arthritis,
· hemophilia,
· uratosis (podarga),
· disorders causing abnormal growth of bone tissue (bone dysplasia), and impaired blood supply and necrosis of bone tissue in the knee (avascular necrosis),
· knee injury or deformation.
Replacement of the joint is an extreme measure, therefore it is recommended only if non-surgical methods of treatment are ineffective, the pain is not removed and the mobility of the joint does not improve.
The non-surgical method of treatment includes physiotherapy to improve flexibility, mobility and joint strength. Painkillers reduce pain in the joint, allowing them to move more freely, and anti-inflammatory drugs reduce the swelling in the joint, increasing its mobility. Injections of steroids into the joint can temporarily relieve pain and swelling. If you have excess weight, then its loss will reduce the burden on the knee joints, the pain will decrease and the mobility will increase.
Replacement of the knee joint may be recommended for adults of all ages, however, in young physically active people, the replaced joint is more likely to wear out. As a result, these operations are usually recommended for older people, they are less active and there is less likelihood that the replaced joint will have to be replaced. Most people who completely replace the knee joint between the ages of 60 and 80. They should tolerate radical surgery and the postoperative period. Recently, in young and more active people with a knee joint replacement, the results improved, and the implanted joints last for 20 years or more.
The operation for prosthetic knee joint is made with general or spinal anesthesia - when you do not sleep but do not feel anything in the lower part of the body, starting from the waist. Typically, the operation takes from one to three hours. Sometimes, together with anesthesia, a nerve block is applied, which relieves pain in the leg within 36 hours after the operation. The knee is opened with a long incision and the patella is exposed. The patella moves, revealing the knee joint, located behind it between the tibia and femur. All bony growths are removed, and the tension of the soft tissues is relaxed, so the knee returns to its natural form.
Damaged parts of bones are removed. This is done with great accuracy, so that precisely fitted components of the artificial joint (prosthesis) can close worn cartilage. The lower end of the femur is replaced by one, an anatomically adapted steel prosthesis. A flat plate of steel or titanium replaces the upper part of the tibia. Plastic inserts are attached to the plate allowing the bones to move easily. Plastic liners are made of polyethylene and therefore they are durable and smooth. Thanks to a combination of metal and plastic, the joint has a low coefficient of friction.
When your bone is measured and prepared, a prosthesis model is put and the joint is tested for stability and correctness of movements. Then it is finally adjusted, the ends of the bones are cleaned and the prosthesis itself is replaced, fixing with a special bone cement, or using a cement-free fixation "press-fit". Then the wound is sutured and bandaged. A tire can also be applied to keep the foot still. After the operation for a while, antibiotics can be prescribed to exclude the development of infection and pain medications are given for pain relief.
Minimally invasive surgery for complete knee replacement
Currently, a new knee replacement technology is available, called minimally invasive surgery (MIS). This technology allows to make the incision smaller in size, up to 10-12 cm, while in the usual method the incision reaches a length of 20-30 cm. A small incision means that a smaller amount of tissue will suffer during the operation. This in turn means that the scar will be smaller, shorter stay in the hospital and recovery after the operation will be faster.
Partial knee replacement
If only one side of the knee is affected, a partial replacement of the knee joint (single-pole replacement of the knee joint) is possible. This is a more gentle procedure than full joint replacement and implies a faster recovery period. However, there is a high probability that in the future, after this procedure, one more operation will be required, which is less likely with a full replacement of the joint. And this means that this operation is less suitable for young active people and is best suited for elderly, lean people who lead an active lifestyle.
Recovery after surgery
As a rule, after the replacement of the knee joint may be painful. Most patients who underwent knee replacement surgery noted that postoperative moderate pain does not compare with the pain they suffered before the operation. The pain can be treated with medicines and gradually passes for several months.
Immediately after the operation, you are prescribed drugs that relieve pain. The day after the operation, a physiotherapist will meet with you, who will explain what exercises to do in order to speed up the recovery.
The physiotherapist will observe and control the recovery process, show exercises for the knee, so that it can be restored more quickly. To restore the motor function in the knee and leg, the physiotherapist can use CPM (prolonged passive movement) by the knee rehabilitation system. This system supports the knee, slowly moves it while you are in bed, reduces the swelling due to keeping your foot up, and improves blood circulation, thanks to the movement in the muscles of the leg.
We recommend walking with a frame or support; over time they are replaced by a cane. Many people start walking alone with a cane in about a week. The wound remains closed and requires regular dressing until complete healing. Stitches or staples will be removed a few weeks after the operation.
Depending on the process of recovery, most people leave the hospital in 7-10 days. Walking is recommended with a cane for a period that is determined by the doctor after discharge from the hospital (usually about 6 weeks after surgery). The physiotherapist will continue to give advice on the development of the knee.
Exercises recommended by a physiotherapist are a key part of rehabilitation, so it is very important to fulfill them. A typical rehabilitation program includes small walking tours to improve mobility, doing ordinary housework, sitting and walking up and down stairs, and special exercises that are performed several times a day to restore mobility and strengthen the knee.
Depending on the progress, the usual life that you conducted during your free time is possible between the third and sixth weeks after the operation. Before the pain stops and the swelling recedes, it can take more than three months, and in your knee the recovery process will continue for another two years if you work on it further and continue to perform the recommended exercises. Further follow-up is a survey every two years.
Driving a car can be resumed when the knee can bend enough to easily get in and out of the car, and when muscle control is restored sufficient for normal driving. Most people are able to get behind the wheel after 4-6 weeks after replacing the knee joint.
Risks associated with knee replacement.
Like any surgical operation, the replacement of knee joints can be associated with certain risks. Possible complications associated with replacement of the knee joint:
· infection of the wound - usually it is treated with antibiotics, rarely the wound is deeply affected, and additional surgical intervention may be required, even more rarely a complete removal of the knee joint,
· fracture or fracture of the bone around the artificial joint during or after surgery - treatment depends on the location and size of the fracture or fracture,
· excessive bone formation around the prosthesis, which limits the movement of the joint - requires additional surgical intervention to remove excess bone tissue and restore joint mobility,
· the formation of excess scar tissue, and as a consequence, the limitation of joint mobility - surgical intervention removes excess tissue, and restores the mobility of the joint,
· displacement of the patella - restoration of its normal position is possible by surgical means,
· numbness around the scar,
· unexpected bleeding in the joint, and damage to the ligaments, arteries or nerves around the knee joint.
In some cases, the knee joint may remain unstable, and additional surgical intervention will be required to adjust it. Within six weeks or more after surgery, blood clots (thrombosis) can form in the veins of the leg, causing pain and swelling. By getting rid of blood clots to means blood-thinning drugs, and usually the problems they do not deliver, but about one person out of twenty there is pain and swelling. Very rarely a clot may come to light, and block a blood vessel (pulmonary embolism), it requires immediate medical attention.
More detailed information about the operation and endoprostheses can be given during the visit of doctor.